The Pathophysiology of OCD: A Deep Dive
These days everyone seems to claim to be a “little OCD’’. Whether it’s a mom who likes to arrange her living room in a specific way or the college student who must color-code her notes for her freshman Chemistry class. There’s a rampant trend of misinformation surrounding OCD. Normal human uniqueness, or simply caring about things, is harmfully characterized as OCD. However, for those genuinely living with OCD, the reality is far more bleak.
What is OCD:
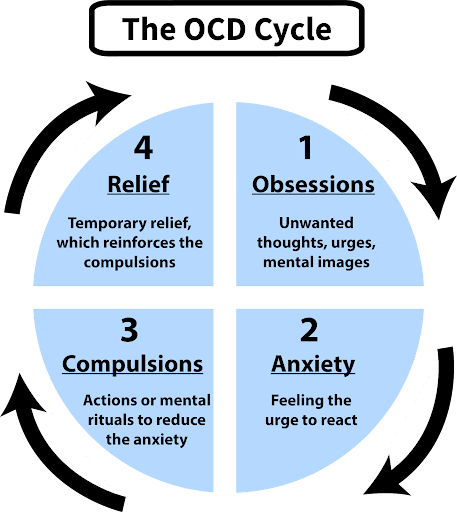
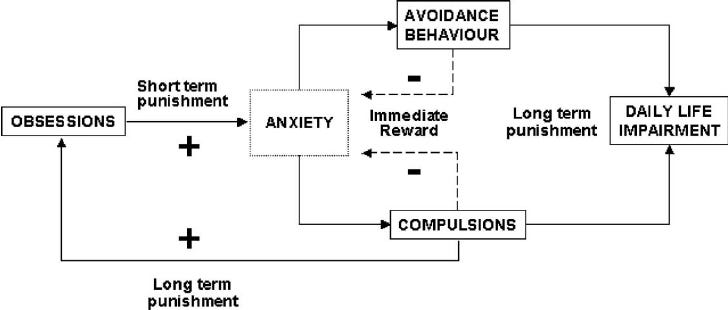
Obsessive-Compulsive Disorder(OCD) is a mental disorder characterized by patterns of obsessions and compulsions. Unwanted and uncontrollable thoughts are known as obsessions while compulsions are repetitive behaviors as a result of the obsession. Compulsions are performed to temporarily relieve the anxiety, but ultimately perpetuate the harmful cycle of OCD.
The Important Brain Structures:
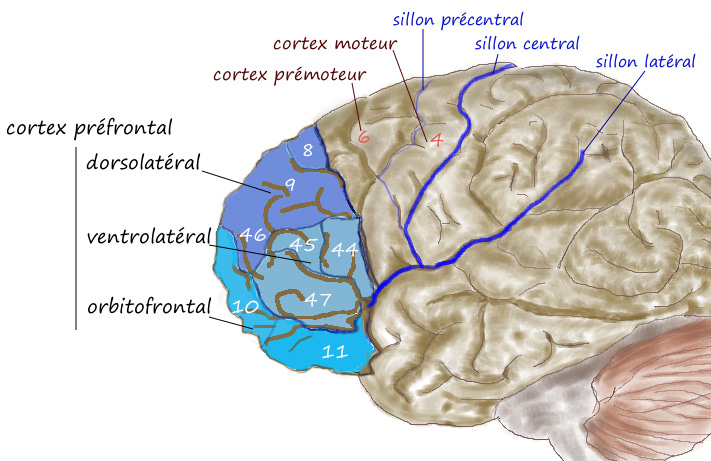
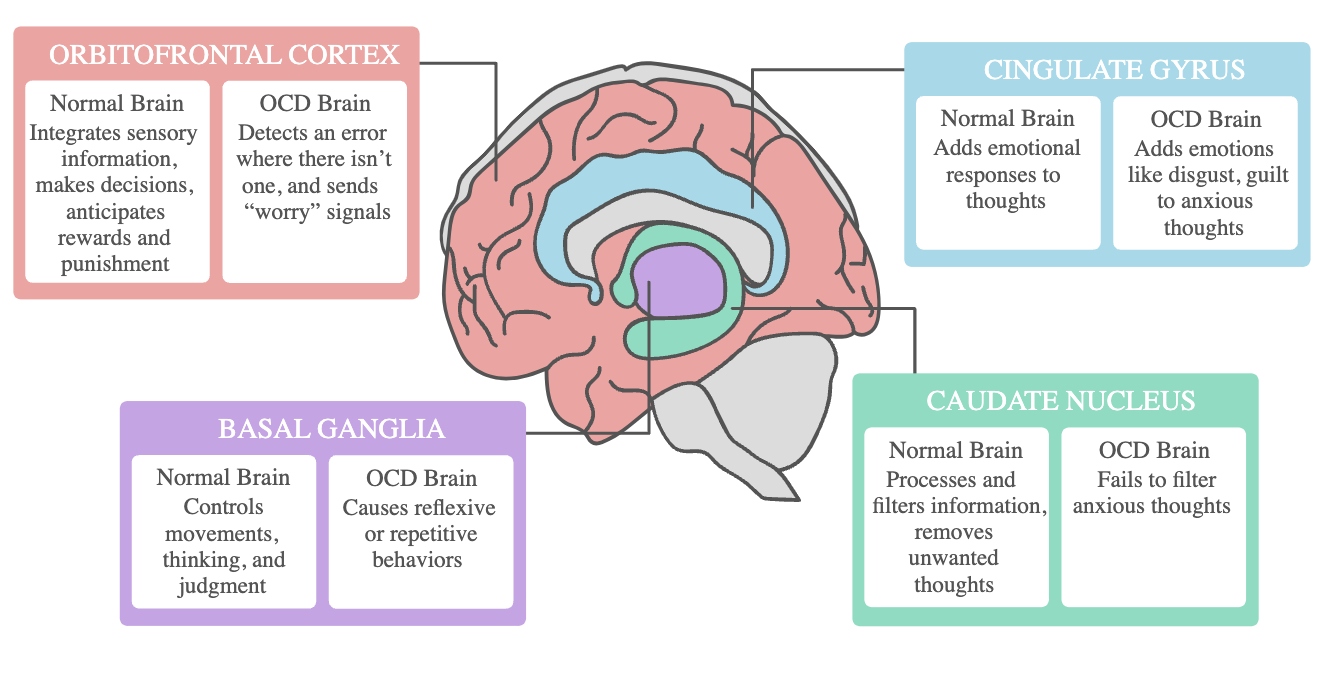
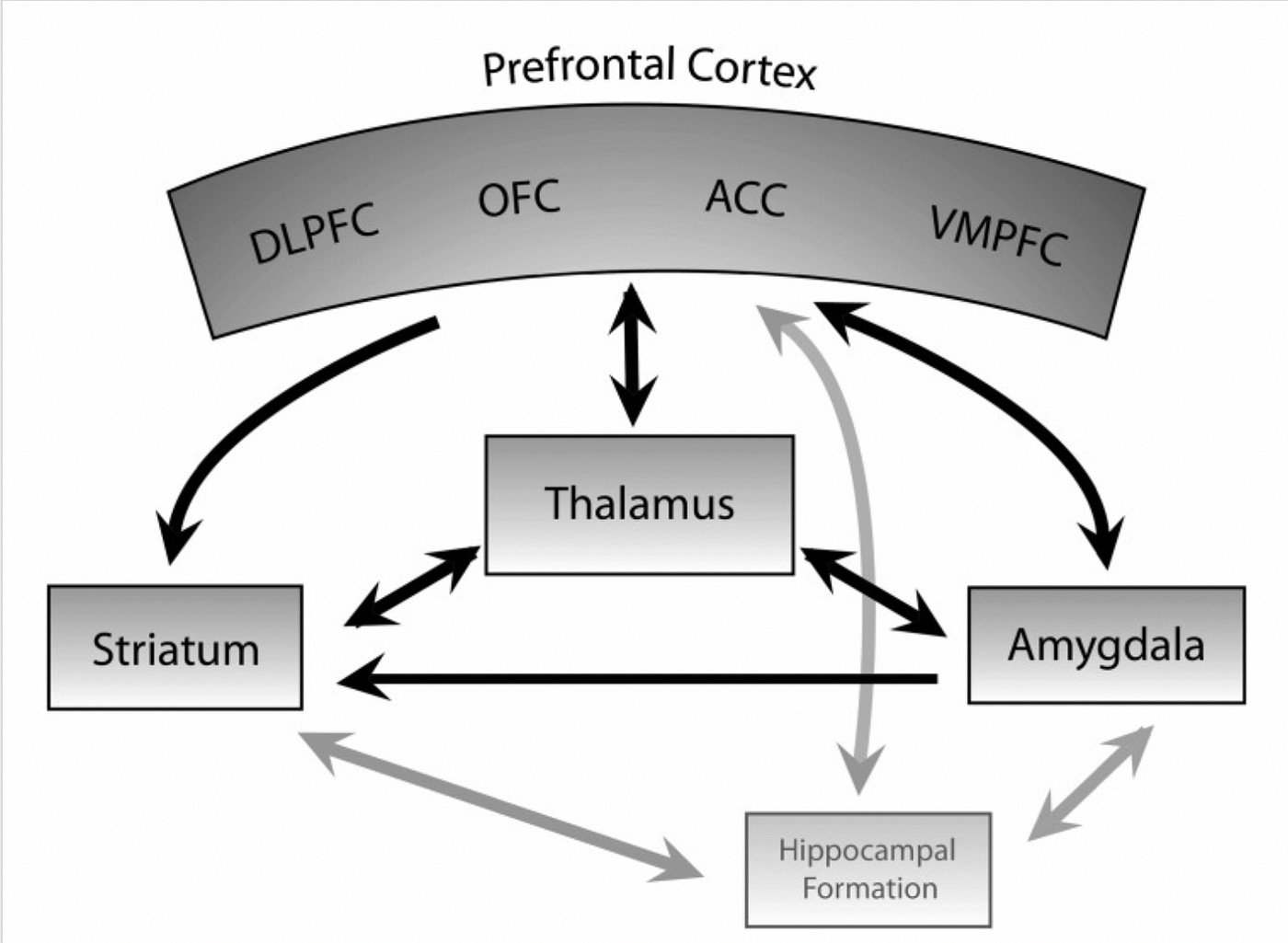
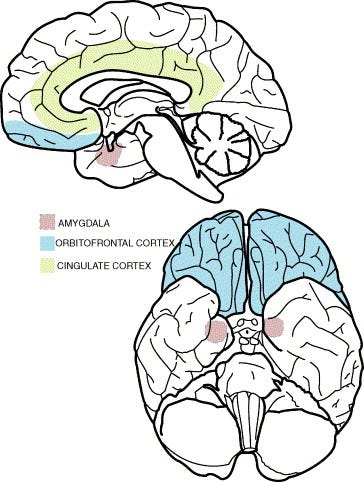
Orbitofrontal Cortex(OFC): It consists of the ventral surface of the frontal lobe. It’s important for decision making by comparing relative value(rewards/punishments) and plays a role in the internal reward system. It also works with the limbic system to regulate emotional processing. In an OCD brain, the OFC detects an error where there isn’t one and sends “worry” signals.
Anterior Cingulate Cortex(ACC): It’s the frontal part of the cingulate gyrus and forms a collar around the corpus callosum. It’s critical to reward anticipation, decision-making, empathy, and emotion. It also regulates autonomic functions such as heart rate and blood pressure. It is a component of the limbic system. In the OCD brain, it adds emotions like disgust and guilt to anxious thoughts.
Amygdala: It’s part of the limbic system, and the major processing center for emotions. It’s critical for behavior, emotional control, and learning. It’s an almond-like paired structure within the temporal lobe.
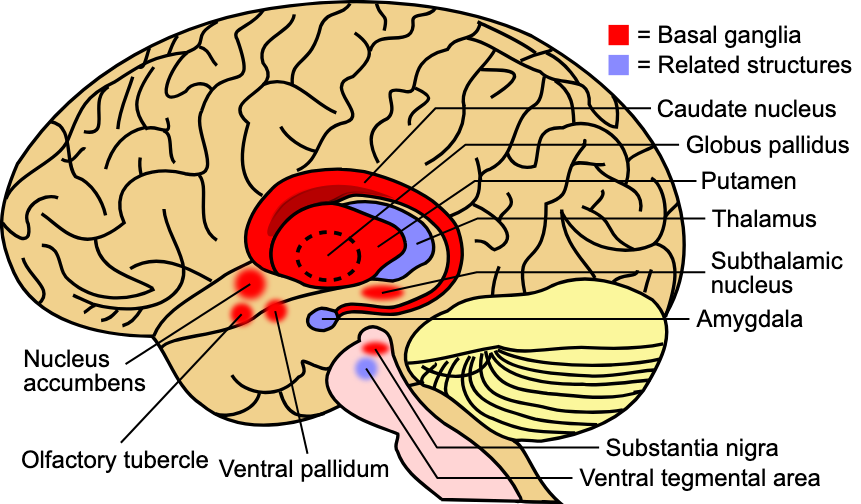
Basal Ganglia: It controls the body’s voluntary movement. It can approve or reject movement signals that your brain sends, filtering out unnecessary or incorrect signals. It also processes how you evaluate goals/risks, so it processes signals that affect emotion and motivation. It is a group of linked structures(Everything in red in diagram below). In the OCD brain, it causes reflexive or repetitive behaviors.
Caudate Nucleus: It is a paired, C-shaped subcortical structure that lies deep inside the brain near the Thalamus. It processes visual information, movement and memory. It plays a vital role in how the brain learns by storing/processing memories. In an OCD brain it fails to filter anxious thoughts.
Substantia Nigra: It releases dopamine that projects to the caudate nucleus. It modulates motor movement and reward functions as part of the basal ganglia circuitry.
Thalamus: It’s the relay station for motor/sensory information from body to brain. All information must pass through the thalamus before being routed to the cerebral cortex. The thalamus is important for prioritizing attention.
Hypothalamus: It maintains homeostasis, directly influences ANS and manages hormones. It’s the main link between the endocrine system and nervous system, and manages blood pressure, hunger, thirst, sex drive.
Striatum: It is a cluster of interconnected nuclei that is part of the basal ganglia. Drug and behavioral addictions affect the plasticity of the striatum. It has been implicated in mediating low levels of motivation in psychopathologies such as schizophrenia and depression. Consists of Caudate Nucleus, Putamen, and Nucleus Accumbens.
Nucleus Accumbens: Nucleus Accumbens is part of rewarding experiences and reinforces addiction/behavior. NA receives fibers from dopamine rich VTA in the midbrain. This is part of the mesolimbic dopamine pathway.
Dorsolateral Prefrontal Cortex(DLPC): It’s critical for cognitive control. It’s involved in overriding prepotent emotional biases, such as when delaying gratification or making utilitarian decisions in the context of moral dilemmas.
The Structural Theories behind OCD:
There are currently many different theories behind the pathophysiology of OCD. However, the prevailing ones seem to share the same brain regions with slight alterations in the relative impact of each region. They all refer to the dysfunction of the loop connecting limbic areas of the prefrontal cortex (orbitofrontal and cingulate) and basal ganglia through the medial thalamus.
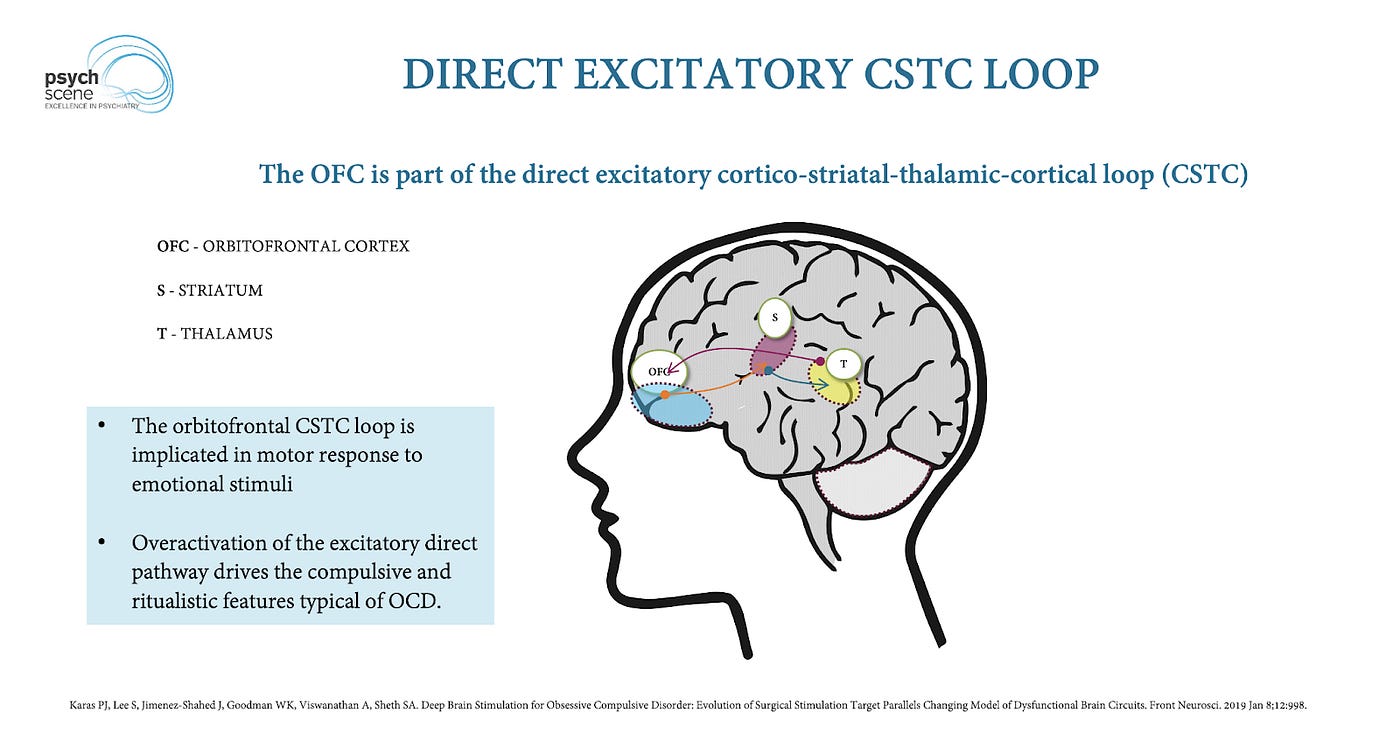
Cortico-Striato-Thalamo-Cortical(CSTC) Circuit Dysfunction Theory:
The specific neuronal loop runs from the orbital frontal cortex to the cingulate gyrus, striatum (caudate nucleus and putamen), globus pallidus, thalamus and back to the frontal cortex. A prominent theory is that OCD involves hyperactivity in specific cortical and subcortical regions. Through a system of positive feedback the hyperactivity is maintained within this circuit. For example, excessive activity in the head of the caudate nucleus inhibits globus pallidus fibers that ordinarily dampen thalamic activity. The thalamus activity is consequently increased and it produces increased activity in the OFC. The cingulate gyrus then acts as a bridge in the circuit from the OFC to the caudate, leading to increased activity in the head of the caudate nucleus. The resulting excess in thalamic output impinges on various brain regions involved in the experience of OCD symptoms, including OFC, reinforcing hyperactivity. It’s worth noting that the impairment of the Caudate Nucleus also allows “worry” inputs from the OFC to excessively inhibit the inhibitory output from the globus pallidus on the thalamus.
This circuit theory, also known as the CSTC Circuit dysfunction theory, is further supported by the result of surgical procedures. It was found that surgically interrupting this loop through cingulotomy, improved symptoms in a large portion of patients that were unresponsive to all other forms of treatment. Through cingulotomy, the loop is interrupted at the ACC, disrupting frontal cortical input into the Papez circuit and Limbic system, reducing feelings of anxiety/negative emotions. The Papez circuit includes the hippocampus, mammillary bodies, anterior thalamus, and cingulate gyrus, and plays a significant role in emotional expression. The reduction in input from the frontal cortex to the limbic system can decrease the intensity of emotional responses and lessen symptoms such as anxiety.
Another brain region implicated in OCD is the Dorsolateral Prefrontal Cortex(DLPC). It is critically involved in cognitive control, particularly in overriding emotional biases and making complex social decisions by balancing emotional and deliberative processes. In OCD response inhibition is severely impaired, and this is linked to dysfunction in the DLPC. A study on Vietnam War veterans who had suffered penetrating brain injury to the DLPC found that damage to the DLPC was associated with repetitive compulsive behavior(Fremont et al. 2021). Another study applied intensified electrical stimulation(tDCS) to the left dorsolateral prefrontal cortex(Molaei et al. 2024). The result was a significant reduction in OCD symptoms and anxiety and depressive states following the intervention. Interestingly, increased connectivity in higher frequency bands at frontal-central areas were observed after treatment and an increase in alpha oscillatory power. An increase in alpha power typically indicates a relaxed state and reduced levels of anxiety.
Striatum Theory:
The ventral striatum’s limbic region is involved in reward-driven learning processes, while the dorsal striatum appears to be responsible for learning semi-conscious behavioral rituals and routines. The theory suggests that disrupted “readiness” and “release” functions of the striatum could lead to OCD symptoms. The readiness and release functions of the striatum are critical for balancing preparation and execution. Dysfunction results in difficulty adequately preparing for actions or anticipating appropriate responses, leading to anxiety or indecision. It may also cause challenges in regulating emotional expressions, leading to emotional responses that are disproportionate to the context or situation.
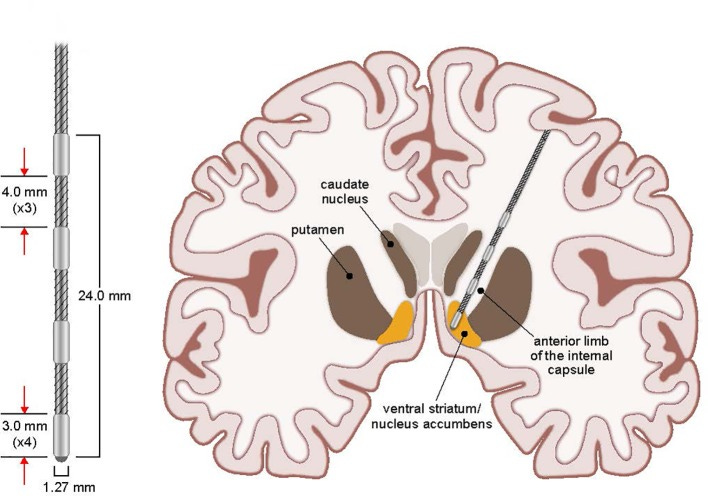
Studies have consistently shown altered functional connectivity between striatum and prefrontal regions in OCD patients. It is hypothesized that dysfunction in the striatum is critical to the emergence of OCD symptoms. A 2009 study found that following treatments, SSRIs and Cognitive Behavior therapy(CBT), neuroimaging reported differentially decreased activity in the striatum and associated cortical regions. Additionally, DBS targeting the ventral striatum region and anterior caudate nucleus, elicited a significant reduction in symptoms in over 50% of patients. During DBS surgery, a neuronal single-unit recording was performed, revealing abnormally high firing rates and variability of MSNs in the caudate nucleus of OCD patients during the expression of symptoms. MSNs are the primary projection neurons in the striatum. A 2010 study introduced OCD gene mutations to mice models and found decreased striatal volume and dysfunctional corticostriatal synaptic transmission. Another study on normal mice found that optogenetic stimulation of the medial OFC, activated the orbitofronto-striatal pathway, leading to the emergence of compulsive behavior accompanied by sustained increases in the activity of MSNs. A key factor of all these studies is the overactivation of striatal circuits.
The Habit Hypothesis:
The habit hypothesis of OCD reflects dysregulation of neural processes, favoring the expression of routinized, habitual sequence of actions triggered by environmental stimuli(Burguiere et. al 2016). These would essentially be considered compulsions in response to distressing stimuli. These behavior routines can be marked by action boundary signals in the striatum and PFC. Within the striatum, neural beginning-and-end signals are distinctly marked by specific patterns of oscillatory/spiking activity. A recent study involving 70 OCD patients suggests that a dysfunction related to the termination of action could excite the patients’ symptoms. If the brain does not properly signal that an action has been completed, individuals may feel compelled to repeat the action until they receive a satisfactory sense of completion. The inability to terminate actions effectively can contribute to increased anxiety and distress, as individuals feel unable to move on from compulsive behaviors. Avoidance behaviors are often a prominent feature in OCD, as patients attempt to avoid situations and stimuli that provoke obsessions, distress, and time-consuming rituals. A study focused on avoidance behaviors in OCD found that participants with OCD repeatedly engaged in avoidance behaviors in response to an external stimuli signaling negative outcomes, even when being told the outcome will no longer depend on their action. The desire for compulsive checking is another central habit to OCD. Compulsive checking may proceed from maladaptive goal-directed behavior toward uncertainty reduction or, in the context of habit-driven behavior, it may result from a failure to control impulses to check.
Stimulus-related uncertainty is encoded in the spike rate of OFC neurons. It’s possible uncertainty-monitoring signals reach the striatum and participate in the regulation of goal-directed behavior, although this is speculative.
The Neurotransmitter Theory:
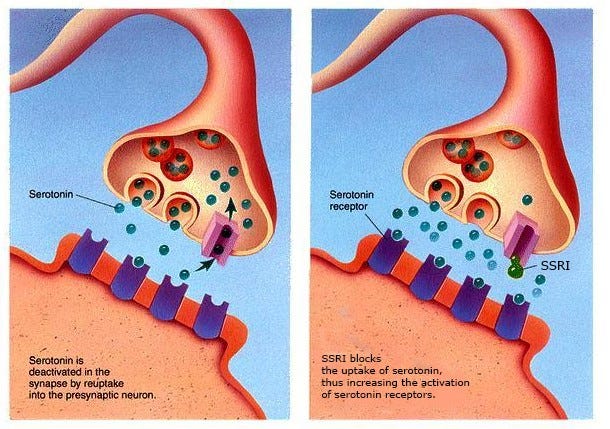
#1: The primary chemical hypothesis for the incidence of OCD is a dysregulation of Serotonin in the brain. Specifically, OCD sufferers typically have a deficiency of serotonin. The importance of serotonin was realized when clomipramine, an antidepressant and SSRI, was found to relieve OCD symptoms. SSRIs work by blocking the uptake of serotonin into neurons,increasing the level of serotonin in the brain. The combination of hypersensitive serotonin postsynaptic receptors and hypoactive presynaptic receptors in OCD patients, leads to dysregulated neurotransmission. A study involving serotonin agonists found behavioral hypersensitivity and neuroendocrinological hyposensitivity to the activation of serotonin receptors(Kellner et al. 2010). Treatments like SSRIs that increase serotonin availability can still be effective because they help normalize the overall system’s activity. Over time, the continuous presence of elevated serotonin levels leads to a decrease in the sensitivity of postsynaptic serotonin receptors. However, whether or not Serotonin is a primary cause versus simply having an involvement in OCD is still up for debate. Serotonergic neurons modulate the function of many other systems, where the primary cause or causes may lie. Additionally, despite the proven efficacy of SSRIs and clomipramine in OCD, about 40% to 60% of patients show no or just partial symptom improvement to a treatment with a first-line drug.
#2: Another emerging theory is the importance of glutamate and GABA in OCD. Glutamate is an excitatory neurotransmitter important for regulating mood and controlling learning and memory. GABA is an inhibitory neurotransmitter, which lessens a nerve cell’s ability to receive, create or send chemical messages to other nerve cells. Imbalances between these excitatory and inhibitory neurotransmitters may provide an environment for compulsions and intrusive thoughts. A 2023 study utilizing magnetic resonance spectroscopy found an imbalance between glutamate and Gaba levels in 31 patients with OCD in the frontal regions of the brain. OCD patients had increased levels of glutamate and lower levels of GABA in the ACC, potentially leading to hyperactivity. Additionally, they found a correlation between clinical severity of compulsive symptoms and glutamate levels measured in the supplementary motor area(Biria et al. 2023). The SMA is important for the coordination of motor sequences and is potentially implicated in habit formation. Glutamatergic modulation might offer novel perspectives in understanding the pathophysiology of compulsivity(Karthik et al. 2020). A study of genetically engineered mice exhibiting corticostriatal dysfunction and OCD-like behaviors, had a dysfunction of glutamatergic signaling within the striatum as a major contributor to the OCD-like behaviors. Re-balancing glutamate and GABA in critical brain regions may lead to a breakthrough in OCD treatment.
I heavily incorporated information and theories from these sources and research papers so please check them out!